Dissociation Across Narcolepsy’s Core Dysfunctional REM Symptoms
The word “dissociation” carries weight, and I hesitated to use it at first. But the more I reflected on my own experiences living with narcolepsy—and the more I read about others’ perspectives—the more the term seemed to fit.
This realization came after an interaction with someone online who was struggling to recognize her cataplexy for what it truly was. Despite already being diagnosed with Type 1 Narcolepsy and having gone through detailed conversations with her doctor about cataplexy, she still found herself uncertain about how it presented in her own body.
I shared a range of descriptions I often use when discussing the different severities of cataplexy—minimal, moderate partial, and severe complete. I explained how the stronger the episode, the more overwhelming the inner sensations become; how maintaining stability becomes an internal battle while remaining engaged with the present and actively participating in whatever one is doing grows increasingly difficult.
That’s when she responded by describing her experience as a dissociation, asking if that was what I meant. Her phrasing sparked something in me—it led me to contemplate the terminology in a way I hadn’t before.
As I explored the term further—reading definitions, analyzing others’ descriptions—it became clear that dissociation presents itself in different ways and at different intensities. And these variations extend across the symptoms of narcolepsy. Whether or not my interpretation of dissociation aligns with the way the term is clinically used in psychology and psychiatry, I can’t say for certain. But I do believe it represents something deeply real—particularly when symptoms reach a certain level of severity.
In ways that may not be immediately obvious, dissociation seems intertwined with narcolepsy’s core symptoms, shaping the lived experience of those navigating the condition.
What is Dissociation?
At its core, dissociation is a disruption in how a person experiences themselves in relation to their surroundings. It can be as simple as zoning out during a conversation or as overwhelming as losing touch with awareness altogether.
Dissociation might be described as:
- Feeling like your brain went “somewhere else” for a few moments, even though you’re still sitting right where you are.
- Being present in class but feeling like you’re watching yourself from a distance, as if your thoughts aren’t quite connected to your body.
- Getting lost in a daydream so deeply that when you snap out of it, it takes a second to remember where you are.
- It’s like your brain is a radio, fully tuned into your own station—strong, clear, fully aware and conscious internally. But as your focus locks onto maintaining steadiness and stability, the external signals flicker out—not fading, but cutting in and out, intermittently distant, as if the connection to the outside world struggles to hold.
It’s not just an experience of losing focus—it’s an altered connection to presence and participation, sometimes momentary, sometimes lasting longer.

The Messiness of Terminology
When discussing narcolepsy and dissociation, terminology often creates confusion. Words attempt to define symptoms, but experiences rarely fit neatly into rigid categories.
Some people might describe an episode in a way that doesn’t align with the terms another person uses. The words chosen might be influenced by how symptoms were first introduced to them, how medical literature frames them, or even how the person personally processes their reality. This misalignment can lead to frustration, misunderstanding, and sometimes defensiveness—especially when discussions challenge or contradict another’s lived experience.
Very rarely are medical descriptions intended to be wide open for interpretation, yet in conditions like narcolepsy, the reality is that much remains unknown—not just about sleep, but about consciousness, cognition, and emotion itself.

Sleep Attacks: The Disappearing Consciousness
Sleep attacks, commonly linked to Excessive Daytime Sleepiness, are far more than just feeling overwhelmingly tired. They are moments where wakefulness battles against unconsciousness, often integrating elements of hypnagogic/hypnopompic hallucinations (HH) and sleep paralysis (SP).
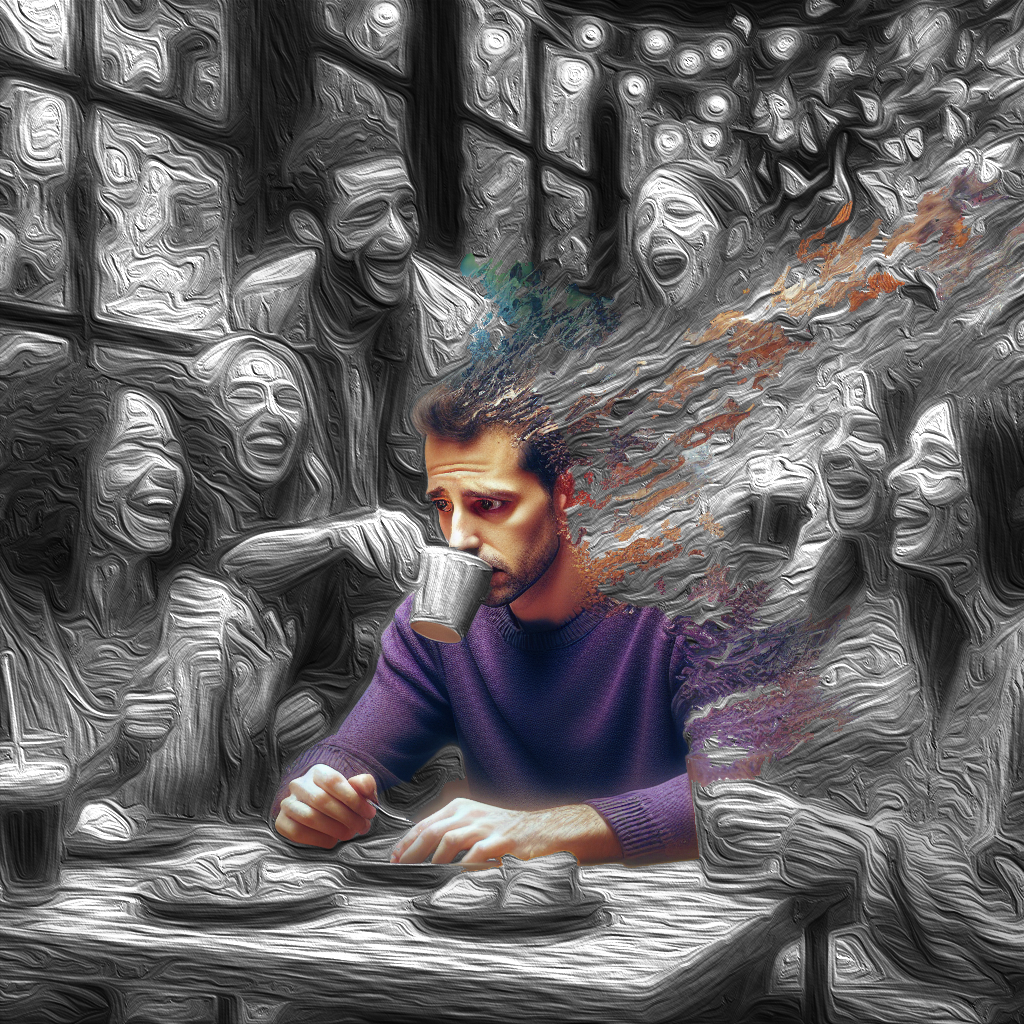
One might drift in and out of REM, slipping between dreaming and wakefulness. Automatic behavior may take hold; brain fog, sleep inertia, and muscular weakness might weigh down the body. A person experiencing a sleep attack can seem drugged—slouching, nodding off—but this state isn’t always apparent to an outside observer.
Internally, dissociation is rampant. A person may be cognitively unreachable, lost in an abyss, absent yet present. They may only realize it happened once they snap out of it—disoriented, discombobulated, struggling to grasp where time just went.

Hypnagogic/Hypnopompic Hallucinations: The Slipping Border
This symptom is often reduced to mere auditory or visual hallucinations, but in reality, it represents something deeper—the fragile barrier between wakefulness and REM sleep.
The experience of HH is intrinsically tied to dissociation. It’s not just hearing things or seeing phantom imagery—it’s the cognitive state of near-dreaming while still physically awake. Reality and dreams intermingle in strange ways, and vigilance wavers, leaving perception fragmented.

Sleep Paralysis: A Spectrum of Cognitive and Physical Detachment
Sleep paralysis is classically defined as a complete muscle paralysis upon waking, yet my experience tells me it’s more nuanced.
Healthcare professionals rarely acknowledge partial extents of this symptom. However, I see it existing on a spectrum—minimal, moderate, and severe. The lesser forms don’t necessarily involve full muscle paralysis, but they do bring physical heaviness, cognitive fog, sleep drunkenness, confusion, and sometimes distress.
These experiences often overlap with HH. A nightmare during HH could even trigger cataplexy, temporarily robbing the body of muscle tone, leading to an unsettling fusion of symptoms.
Cataplexy: The Internal Battle
Dissociation within cataplexy is different. While other symptoms may steal cognitive awareness, cataplexy centers around maintaining control in the face of complete bodily collapse.
The urgency to remain steady is overwhelming. Inside, the body feels waves of flickering sensations—muscles twitching, rushes moving through the head and limbs. Time may feel still, external focus distant.
For example, continuing to actively listen and absorb what is being said becomes difficult. Thoughts don’t stop, but the gears of the mind stutter—grinding in a way that makes remaining fully engaged subtly to fiercely challenging. As one’s energy and focus become overwhelmed by the effort to remain physically stable—to not outwardly appear as though something is failing—the mind also struggles under the weight of that interference. One might compare it to the sensation of butterflies during strong moments of anxiety, a nervous flutter in the stomach. But here, the interference is something far greater—where the physical glitches, short-circuits, and twitches out, the cognitive battle is not a butterfly but an eagle, massive and consuming, commanding attention whether one wants it or not.

A Personal Understanding
Dissociation across narcolepsy is vast, fluctuating, and highly individual. It shifts from person to person, symptom to symptom, moment to moment.
No two experiences are identical in expression, but the deeper patterns are undeniable. Language may differ—terms may not overlap—but at their core, these experiences hold striking similarities across those living with this disease.
Dissociation within narcolepsy isn’t just an abstract concept—it’s a lived reality, often unrecognized, yet deeply felt.

————————————————————————————————————————————————————————-
Disclaimer: The information provided in this article is intended for informational and educational purposes only. Seek a qualified medical professional with expertise in Narcolepsy for diagnosis or treatment. I am not a medical professional.
Created by Solomon Briggs
(aka Narcoplexic)
May 8th, 2025
A Flickering Reality: The Unseen Dissociation Within Narcolepsy © 2025 by Solomon Briggs is licensed under Creative Commons Attribution-NonCommercial 4.0 International
To view a copy of this license, visit https://creativecommons.org/licenses/by-nc/4.0/
“You may use this tool for non-commercial purposes, but must credit Solomon Briggs.”

Katy Blasdell May 12, 2025
You have put into words how narcolepsy feels. I appreciated this article very much. I have been living with this disease for most of my adult life; although, I wasn’t properly diagnosed until I was 36. I do have narcolepsy type 1. Dealing with the sleep paralysis, the hypnogogic hallucinations, sleep attacks, automatic behavior, and the cataplexy does feel as though you are dissociated with reality for sure. Trying to balance and reconcile that in your life gets to be a little on the verge of craziness. Before my diagnosis I thought I might be going insane.
sol.briggs May 16, 2025 — Post Author
Thanks for commenting! Am glad to articulate it in a way that you could relate to. Trying to bring some clarity to the lived experience.