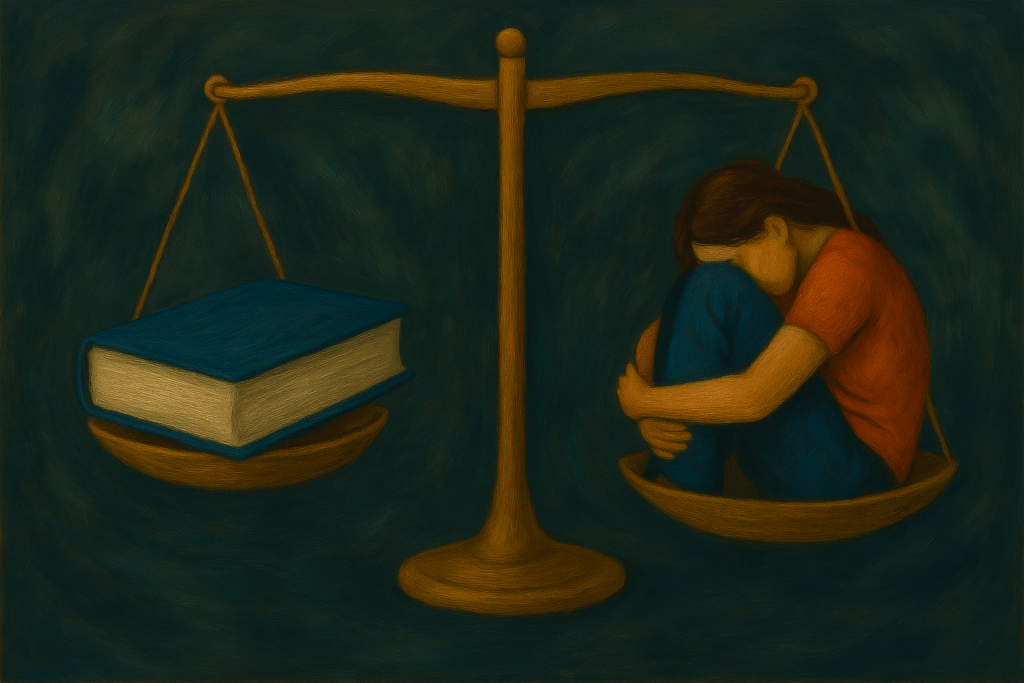
Living with Cataplexy: Bridging the Gap Between Understanding and Experience
When you live with a condition as rare and misunderstood as Cataplexy, especially its moderate partial to severe complete manifestations, life becomes a constant balancing act. For those of us dealing with Narcolepsy Type 1 (N1), the spotlight often falls on the exhaustion and sleep attacks associated with this condition. However, Cataplexy—a sudden, uncontrollable episode of muscle interference to what can be a temporary complete muscle paralysis, triggered by strong emotions or exhaustion, in rare cases—is frequently misunderstood, even among medical professionals and fellow N1 sufferers.

The Misunderstood Symptom
The challenge with Cataplexy lies partly in its terminology. It is clinically defined as a loss of muscle tone, often referred to in medical contexts as “muscle weakness,” ranging from minimal partial effects to temporary complete muscle paralysis. These episodes, triggered by emotional stimulation—laughter being the most commonly recognized trigger—occur while the individual remains fully conscious. However, the description of “muscle weakness” fails to capture the reality of what Cataplexy entails. This terminology is not only misleading but oversimplified, as it reduces a profoundly disruptive condition to something that sounds far less impactful. A more accurate description would frame it as “muscle interference” or “muscular interferences,” reflecting the disruptions to muscle function and control that define this symptom.
For many, Cataplexy is mistakenly conflated with sleep attacks or seen as a quirky reaction to laughter or joy. But for us, the reality is far more complex. While laughter is often the most commonly recognized trigger, Cataplexy episodes are not solely tied to emotions. Exertion of physical, mental, or social energy can also act as a catalyst, particularly when we are already stretched beyond our limits.
Adding to this confusion is the fact that “muscle weakness” is genuinely experienced during states of sleepiness and during sleep attacks. This overlap creates a vast misunderstanding of what Cataplexy truly is, blurring the lines between different symptoms of Narcolepsy. The term “muscle weakness,” though commonly used in medical contexts to define Cataplexy, contributes to this confusion by inadequately capturing the nature of Cataplexy itself. Unlike the gradual, fatigue-related “weakness” felt during sleepiness, Cataplexy involves sudden and often complete disruptions to muscle control—what should be more aptly described as “muscle interference” or “muscular interferences.”

A Rare Experience in a Rare Disease
Cataplexy, in its more severe forms, adds a layer of difficulty to a condition already defined by its challenges. Living with it feels akin to having a seizure condition layered on top of the other symptoms of N1—excessive daytime sleepiness (EDS), hypnagogic hallucinations (HH), sleep paralysis (SP), and disrupted nighttime sleep (DNS). Beyond that, there’s the brain fog, sleep inertia, and a myriad of other effects that disrupt daily life. Yet, despite these realities, the lived human experience of severe Cataplexy remains vastly underexplored, even within the medical community.

The Science vs. the Lived Experience
While advances in science, like the development of Orexin Agonists, offer hope, they don’t address the full picture. These treatments may improve wakefulness and potentially Cataplexy very much as well, but they don’t yet tackle the complexity of poor sleep quality or the disrupted REM cycles that define our nights. The gap between scientific advancement and lived experience often feels insurmountable, especially when Narcolepsy and Cataplexy are presented as though it fits neatly into a “solved” box.
This disconnect isn’t just frustrating—it’s isolating. The oversimplification of Narcolepsy, and especially Cataplexy, does a disservice to those of us grappling with the anxiety, unpredictability, and sheer life-altering impact it imposes. For now, the narratives surrounding Cataplexy feel more like fleeting clouds than concrete realities. Fluid, not solid.
Learning to Navigate Life with Cataplexy
Living with moderate partial to severe complete Cataplexy requires an ongoing process of learning and adaptation—yet this is rarely emphasized in the medical realm’s approach. Beyond the use of medication, which can help but is not always sufficient, managing Cataplexy truly involves becoming deeply attuned to our own triggers and recognizing severity levels, both ‘in the moment’ and ‘over ongoing moments.’ It’s about understanding the boundaries we must navigate within and finding effective ways to reduce stress and anxiety.
Attempting to fight the onset of an episode often does more harm than good, amplifying and prolonging it. Learning to accept and manage these moments is a journey that takes time, patience, and self-compassion. The anxiety Cataplexy creates is distinct and fiercely intense—a hallmark of the condition. Yet, over time, it is possible to adjust and find ways to coexist more harmoniously with this symptom.
Lifestyle changes, heightened self-awareness, and a profound understanding of Cataplexy—alongside acceptance of our limitations—can, eventually, help ease its overwhelming burden.

Advocacy for Change
For over 15 years, I’ve immersed myself in the medical literature, while engaging in conversations about Cataplexy online. Through lived experience and research, I’ve become a passionate advocate for greater understanding and recognition of this condition; though I feel rarely heard outside of anonymous online interactions where I have received thousands of people saying they feel validated by what I’ve said, as well as people having actually tried very specific methods I’ve mentioned (like getting to the ground when it reaches a moderate point, rather than continuing whatever, battling through it).
We are not “patients” defined solely by our diagnosis; we are individuals navigating an incredibly challenging, life-altering disease. I hate the term patient/s and how it gets used, it is diminishing and can be insulting; but I do get it or the need for the term.
The journey is far from easy. Cataplexy’s impact, coupled with the anxiety that it uniquely creates, remains profoundly misunderstood—even by those who aim to help. But by sharing our experiences and continuing to advocate for greater focus on the human side of living with Narcolepsy and especially Cataplexy, we can begin to bridge the gap that so often leaves us feeling isolated and unseen.

—————————————————————————————-
Disclaimer: The information provided in this article about Cataplexy is intended for informational and educational purposes only. Seek a qualified medical professional with expertise in Narcolepsy for diagnosis or treatment. I am not a medical professional.
Created by Solomon Briggs
(aka Narcoplexic)
April 30th 2025
Beyond Weakness: Muscle Interference and the Fight for Cataplexy Awareness © 2025 by Solomon Briggs is licensed under Creative Commons Attribution-NonCommercial 4.0 International
To view a copy of this license, visit https://creativecommons.org/licenses/by-nc/4.0/
“You may use this tool for non-commercial purposes, but must credit Solomon Briggs.”

Beth Louise Parker May 1, 2025
Solomon, you have really captured what I’ve never known how to explain. Thank you!
sol.briggs May 9, 2025 — Post Author
Thank you! I appreciate your commenting and letting me know my efforts are not going unseen.
Kathie Dees May 13, 2025
Great explanations. Thank you for the awareness.
sol.briggs May 16, 2025 — Post Author
Thank you for commenting!